- What is Thermography?
- Is Thermography Useful in Detecting Breast Cancer?
- What is Computerized Thermal Imaging?
- How Does Computerized Thermal Imaging Work?
- Where is Computerized Thermal Imaging Being Evaluated?
- What are the Limitations to Computerized Thermal Imaging?
- What Imaging Exams are Currently FDA Approved to Help Detect Breast Cancer?
- Additional Resources and References
Thermography (also called thermal imaging or infrared imaging) was approved by the U.S. Food and Drug Administration (FDA) in 1982 as a supplement to mammography in helping to detect breast cancer. Thermography can help determine whether a local abnormality in breast tissue temperature is present, which may indicate the presence of disease. Though thermography is FDA approved, the exam has not gained acceptance in the medical community as a necessary or effective tool in breast cancer detection. According to the American College of Radiology, thermography has not shown value as a screening, diagnostic, or adjunctive imaging tool.
While thermography may be appealing to some women because it is a pain-free exam, most physicians do not recommend thermal imaging. Scientific research over the last 20 years has shown that thermography is not reliable for detecting breast cancer. In 1977, the Beahrs Committee of the National Cancer Institute (NCI) recommended that thermography be discontinued as a routine screening modality in the NCI’s Breast Cancer Detection Demonstration Project.
Since then, studies have failed to show a clear benefit of thermal imaging in helping to detect breast cancer. In their 1998 document, "Evaluation of Common Breast Problems: Guidance for Primary Care Providers," Barbara Smith, MD, PhD and her colleagues wrote, "currently, thermography has no role in breast cancer screening or diagnostic evaluation." Several other reports have drawn similar conclusions. That is not to say that improved thermography technology may not one day aid in the breast cancer diagnostic process (see computerized thermal imaging sections below); however, at the moment, thermography is not widely accepted as an effective means of detecting breast cancer.
 |
Inside view of computerized thermal imaging system with mirrors that deflect infrared waves from a patient's breast to a camera below. Image courtesy of CTI, Inc. |
Computerized thermal imaging (CTI) is a new, non-invasive imaging method that is being developed using the principles of traditional thermography but with the addition of digital image reconstruction. Computerized thermal imaging (CTI) is a heat sensing and processing system that uses a thermal sensitive camera to capture a digital image based on heat radiating from the body. A computer-assisted interpretation of the digital image helps to determine whether a local abnormality in breast tissue temperature is present, which may indicate the presence of disease. To date, CTI is only available for eligible women who participate in CTI clinical trials; the technology has not been approved by the U.S. FDA.
Currently, clinical trials are being conducted at five hospitals across the United States to determine whether the CTI technology may be useful as an adjunct (supplement) to mammography in the breast cancer diagnostic process.
The main component of the CTI technology is the highly sensitive, high-speed infrared camera. The camera is designed to detect infrared heat given off by the body. After the radiologist has acquired images of the breast tissue, the CTI system uses sophisticated image analysis algorithms and a computer to reconstruct the images to show individual heat patterns. These images differentiate between normal and abnormal heat patterns. The CTI examination consists of the patient being positioned on a special examination bed with the breast suspended in an opening in the top of the bed. The thermal camera is located inside of the bed, focused at the examination area. The physician will use the thermal camera to take a series of images of the breast. The procedure is then repeated with the patient’s other breast. As with traditional thermography, no radiation or breast compression is used during CTI.
After the breast images have been taken, they are analyzed by a computer algorithm and displayed for interpretation by the physician. Breast images are displayed in different colors (red, orange, and yellow) on a computer monitor for the physician to review. Any suspicious area (abnormal heat area) is marked on the digital breast image. The radiologist may then decide whether further breast imaging is necessary. The CTI technology is designed to electronically store the digital breast images and provide the patient with an electronic copy of the images, which may be helpful if she visits another imaging facility.
Malignant (cancerous) image:
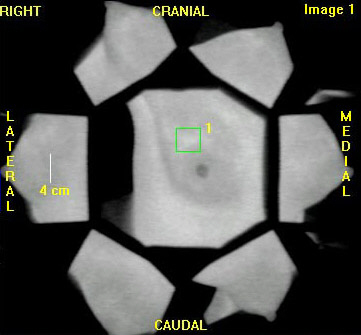 |
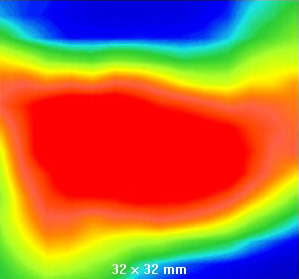 |
The left image is the raw thermal image. The right image is a magnified view of the processed image that corresponds to the area of suspicion selected by the green square in the left image. This image shows a very high probability of malignancy (cancer). This patient was rated a BIRAD 4 (suspected malignancy, biopsy recommended) by mammography and confirmed to have ductal carcinoma in situ by biopsy. Images courtesy of Computerized Thermal Imaging, Inc.



