- Will the MR imaging examination hurt?
- How long will the MR examination take?
- Why does the MR system make the knocking sound during the exam?
- Why may I need to have an x-ray image before my MR imaging exam?
- Will the MR imaging affect the fillings in my teeth?
- Can I have an MR exam if I have braces on my teeth?
- Do I have to go all the way inside the MR scanner tunnel?
- Do I need a referral (prescription) to receive an MR examination?
- Can I move while I am in the MR tunnel?
- Can I talk with anyone during the scan?
- Can I bring a friend or a relative into the MR scan room with me?
- Do I need an injection of contrast for my MRI exam?
- How is the Gadolinium injection given for an MR imaging exam?
- If I'm nursing an infant, can I breast feed after an injection of Gadolinium?
- Can I have an MR imaging exam if I am pregnant?



No, MR imaging itself should cause no pain. MR imaging requires that the patient remain still during the examination. For some patients, keeping still for some time may be slightly uncomfortable. Sometimes patients may feel warmth in the area being imaged, this is normal. However, if this warmth becomes irritating or excessive, the patient should notify the imaging technologist as soon as possible.
MR imaging examinations which require the patient to receive Gadolinium contrast may cause slight, temporary discomfort while the intravenous needle is placed (see below section "do I need an injection").
Most MRI centers offer a wide array of Magnetic Resonance (MR) imaging examinations. Depending on the type of exam you will receive, the length of the actual procedure will typically last between 15 minutes and 45 minutes. A few involved MRI examinations take longer than 45 minutes. Also, some MR exams require the patient to hold their breath several times. This helps to eliminate blurring from the images, which can be caused by breathing or other patient motion. Please discuss specific questions about the duration of your MR imaging examination with the MR technologist before your exam.
The tapping or knocking noise heard during the MR exam is created when "gradient coils" are switched on and off to measure the MR signal reflecting back out of the patient's body. Depending on the type of study being performed, the knocking may be loud enough to require ear plugs or head phones for the patient. Please discuss this with the technologist before your examination. During the MR examination, the technologist and patient may usually communicate at any time via intercom or a type of call button.
The gradient coil is one of several internal parts of the MR system that you cannot see. The gradient coil is made up of loops of wire which are embedded in a hard plastic tube. During the scanning process an electric current is switched on and off through the gradient coil approximately every few milliseconds. Because the switching is so rapid, the wires vibrate within the hard plastic and cause the knocking sound. This knocking is not harmful but the sound can be irritating to some patients. You will here different knocking sounds during the MR exam, this means that different types of "MR sequences" are being run to acquire different views and images of your body.
MR imaging involves the use of a strong magnetic field. This magnetic field pulls on many metal objects. Thus, for safety reasons, the MR staff must determine if you unknowingly have metal in your body. Some patients may have small pieces of metal in their eyes, a metal implant, a prosthetic device that may contain metal, surgical clips or other implanted objects that may be susceptible to the magnetic field. After asking you a few questions, x-ray imaging may be necessary to screen for metallic items prior to the MR examination.
No, MR imaging will not cause fillings in your teeth, if in proper condition, to dislodge or come out. The metal in most fillings is not affected by the MR system's magnetic field. However, the fillings may cause some distortion of the images if you are having a scan of your neck, brain or facial area.
Patients with braces may receive an MR imaging examination. However, if you have braces and need MR imaging of your brain or facial area, the MR system may have difficulty "tuning" to your body. The MR tuning process is similar to tuning a radio to a specific frequency or radio station. This tuning process can be "confused" if the patient has metal in his or her body, particularly if the metal is in the area being imaged. Unfortunately, there is no way to know in advance how much distortion from braces may result on MR images of the head, face or upper neck.
Yes, however, only the portion of the body that is being imaged must be positioned in the middle (end to end and side to side) of the MR system's tunnel or "all the way inside." For example, if a head study is being performed, the patients head must be positioned in the middle of the tunnel. For knee studies, the knee is positioned in the middle of the tunnel with the patients head facing the open end or possibly outside of the open end of the scanner (depending on the length of the magnet tunnel and the height of the patient). So-called "Open MR" systems do not have a tunnel design and may be more comfortable for some patients. Most MR systems use the cylindrical tunnel design; however, recent versions of the cylindrical MR systems have tunnels that are shorter, more open, and more comfortable than systems designed and manufactured previously.
Yes, your doctor must give you a referral (prescription) in order for you to receive a Magnetic Resonance (MR) imaging examination.
You should not move when you are inside the tunnel and hear the knocking sound. For most MR exams, you may reposition your arms or scratch your face or body in between image acquisition, when the knocking has stopped. However, it is important that you not move the body part being imaged until the entire exam is complete. Some MR exams of the chest and abdomen may require the patient to hold their breath for a short period of time, for example, 10 to 25 seconds. This eliminates blurring in the image caused by breathing or other patient motion.
You may talk to the technologists or ask a question in between pictures image acquisition sequences when the knocking has stopped. You will know when a picture is complete because the knocking and slight vibration will stop.
Various MR centers may have different procedures regarding this question (depending upon the type, strength and external shielding of their magnet). All people entering the MR scan room should be checked for metal in or on their body. This check may include the removal of keys, coins, jewelry, watches, hairpins, hair clips, hearing aids, wallets, and credit cards or ID cards with magnetic strips (since the strips magnetic coding can be erased by the magnetic field). From a medical and safety standpoint, if your companion is checked and cleared to enter the MR scan room, he or she may safely accompany you for the exam. Typically your companion will be seated in a chair next to the MR scanner, or they may stand next to the patient table during your exam.
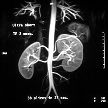
Not everyone needs an injection for MR imaging. When an injection is needed, a pharmaceutical contrast agent called Gadolinium is administered to the patient. This is only done when the radiologist and/or the referring physician have determined that it is necessary for diagnostic purposes. Gadolinium contrast is used to make specific organs, blood vessels or tissue types "stand out" with more image contrast in the resulting picture. This highlights the structure of the specific organs or vessel to better show the presence of disease or injury. The referring doctor provides the MR imaging center with information about the patient's medical condition and the goal of the MR imaging procedure being ordered (for example, to diagnose cause of intense back pain). The decision to use or not to use an injection of contrast (Gadolinium) is made based on this information and the body part being examined.
If an MR exam does require the use of a Gadolinium injection, a small needle connected to an intravenous line is usually inserted into the patient's arm or hand. A special saline solution is first dripped in to keep the vein from clotting. Then typically, about two-thirds through the exam, a contrast agent called "Gadolinium" will be administered through the intravenous line. At the time of the injection, a patient may feel a cool sensation going up his or her arm. As with anything taken into the body, there is a very slight chance of an allergic reaction. For more information on contrast injections, please see the section on General Information About Contrast ("Dye") Used in Medical Imaging Examinations.
Typically, patients are instructed to wait for 24 hours after receiving the Gadolinium injection before breast feeding again. Patients may wish to pump breast milk prior to the MR exam and store it for use during this 24-hour period. Always check with the radiologist and the imaging center for their specific recommendations.
This question is difficult to answer with a simple "yes" or "no." MRI (magnetic resonance imaging) is considered a safe exam. However, conclusive information showing how safe MRI is for pregnant women and the fetus is not yet available. MR imaging is generally not performed on women in the first twelve weeks of pregnancy (first trimester).
Physicians typically do not perform MRI on pregnant women unless there are strong medical indications. Depending on the condition, there may be other exams available, such as ultrasound, to help diagnose a medical condition.
If there is a strong medical reason for an MRI, your physician may consult with a radiologist to determine if MRI is the best course of action before proceeding. An abbreviated MRI exam may be performed, to reduce the time in the magnetic field, based on the recommendation of the referring physician and radiologist. Please consult with your physician for more specific information.



